What is Blood Glucose?
Glucose is a form
of sugar produced when the body digests carbohydrates (sugars and starches).
Glucose is the body's major fuel for the energy it needs. When insulin is
absent or ineffective, the blood glucose (blood sugar) level increases. High
blood glucose levels can lead to both short and long-term problems.
When and why does its level in
the blood change?
Your
blood glucose levels change during the day. Blood glucose levels are affected
by food, exercise, emotions, and insulin. However, you will not always feel
your blood glucose level go up or down. One of the best ways to be certain that
your blood glucose levels are maintained within the Diabetes Safe Zone* is by
regularly self-monitoring your glucose level.
Knowing
your blood glucose levels at different times of the day can help you and your
doctor see how well your meals, activities, medicines and insulin are working
and what action to take.
What is Diabetes? How is it
related to blood glucose level in blood?
Diabetes
is a chronic disease in which the body does not make, or does not properly use,
insulin. Insulin is the hormone that helps your body use the energy from sugar,
starches and other foods. The result is that your body doesn't get the energy
it needs, and unmetabolized glucose (undigested sugar), builds up in your blood
causing damage to the body and its systems.
There
are different kinds of diabetes, each with slightly varying symptoms and
treatments. The principal forms are Type 1 and Type 2. Related conditions
considered to be "prediabetes" include impaired glucose tolerance and
impaired fasting glucose. Pregnant women may develop gestational diabetes.
Women who already have diabetes may also have certain condition-related
concerns during pregnancy with diabetes.
What are the treatments
available for Diabetes?
At
present, no cure is available for diabetes. But with regular self-monitoring of
blood glucose and a proper combination of diet, exercise and medication, people
with diabetes can lead active, healthy lives.
Ways to assess blood glucose levels (A1C)
An HbA1C laboratory test
(also know as a glycated hemoglobin test or HbA1C test) gives your doctor a
picture of your average blood glucose control for the past 2 to 3 months. Your
doctor may regularly perform this blood test at your routine visits. The more
excess glucose in your blood, the higher is your A1C results.
Your A1C does not show daily changes in your blood glucose
|
Two people have the same
A1C of 7.5%, but see
how the swings in blood glucose are different? |
Self-monitoring of blood glucose (SMBG)
Self-monitoring of blood glucose gives your doctor critical feedback in between
your A1C or lab tests about whether the right treatment choices are being made.
Self-monitoring of blood glucose also helps you manage the
day-to-day highs and lows sometimes associated with diabetes treatment. And
because your body and medication needs will naturally change over time,
particularly with insulin, self-monitoring of blood glucose helps you spot
these changes in your blood glucose.
What are the symptoms of
uncontrolled diabetes
When blood glucose levels are
poorly controlled, a person with diabetes can suffer from too much glucose in
the blood (hyperglycemia) or too little glucose in the blood (hypoglycemia). When
this happens, the person could experience symptoms of uncontrolled diabetes.
Symptoms of high blood glucose (hyperglycemia)
These are the symptoms of high blood glucose (hyperglycemia).
Regular monitoring can help you avoid high and low blood glucose, avoid
complications of diabetes, and help control your blood glucose levels.
High Blood Glucose Symptoms
|
Increased Thirst
High blood glucose can cause excessive thirst. If you are always thirsty and
you can't seem to get enough fluids despite the amount you drink, diabetes may
be out of control.
Hunger
When insulin in the body is insufficient to push glucose into the cells of the
body, glucose stays in the blood streams. As a result, your brain detects this
and tells you that you need food.
Headaches and difficulty concentrating
Too much glucose in the blood can result in your brain cells not getting enough
glucose to function properly.
Blurred vision
High blood glucose can cause eye problems. High levels of blood
glucose pull fluid from your tissues, including the lenses of your eyes, making
focusing difficult. If your diabetes is uncontrolled, blood vessels in the
retina are damaged, and new blood vessels form. You may experience mild vision
problems, such as dark spots, flashing lights or rings around lights. It can
also cause blindness.
Frequent urination
High blood glucose can cause frequent urination, one of the
classic symptoms of uncontrolled diabetes. Although it doesn't always signal
uncontrolled diabetes, if you have diabetes and you have to go too often, then
your blood glucose control may be poor. As a result of this, you will feel
thirsty, no matter how much you try to replenish the fluids that you lose.
Fatigue
or tiredness
High blood glucose can cause fatigue. If you are getting regular
exercise, being diligent with your medication, aren't pregnant, or are
relatively stress-free, yet you feel tired and sleepy frequently and have
difficulty getting through the day, your diabetes may be out of control. This
means that your body is storing and using glucose poorly.
Weight Loss
Too much glucose in the blood can result in your body failing to
store glucose in cells properly, and start to break down other sources for
energy instead, resulting in weight loss.
Infections
High blood glucose weakens your body's immunity and defenses against infection. When your blood glucose levels are persistently high, your body's natural ability to heal and fight off infections is impaired. You become vulnerable to influenza, bladder and vaginal infections. If you are always fighting infections, your diabetes may be uncontrolled.
High blood glucose weakens your body's immunity and defenses against infection. When your blood glucose levels are persistently high, your body's natural ability to heal and fight off infections is impaired. You become vulnerable to influenza, bladder and vaginal infections. If you are always fighting infections, your diabetes may be uncontrolled.
Foot Problems
High blood glucose can lead to nerve damage, usually in the
extremities and particularly in the feet and lower leg. You may notice tingling
and loss of sensation or burning pain in your feet, legs and hands.
Other conditions
Other signs of high blood glucose can include dry mouth, dry or
itchy skin, male impotence, vaginal yeast infections, unexplained aches and
pains, urinary tract infections, sores that don't heal very well, excessive
infections and genital itching.
Symptoms will vary from person to person, and may be affected by age or sex.
Symptoms of low blood glucose
(hypoglycemia)
Regular monitoring can help you spot patterns to try to avoid low
blood glucose, reduce complications of diabetes, and help control your
diabetes. Symptoms of low blood glucose (hypoglycemia) may include:
Neuroglycopenia
The main symptom of low blood glucose is impaired brain function (neuroglycopenia). When blood glucose levels are too low, the brain fails to get enough glucose, and it reduces some of the things it normally does. This results in dizziness or light-headedness, sleepiness, confusion, difficulty speaking, and other symptoms.
The main symptom of low blood glucose is impaired brain function (neuroglycopenia). When blood glucose levels are too low, the brain fails to get enough glucose, and it reduces some of the things it normally does. This results in dizziness or light-headedness, sleepiness, confusion, difficulty speaking, and other symptoms.
Hunger
Low blood glucose can result in a feeling of hunger. When glucose levels are too low in the blood as a result of too much insulin, the cells of the body do not get enough glucose, and your brain is triggered to tell you that you need to eat.
Low blood glucose can result in a feeling of hunger. When glucose levels are too low in the blood as a result of too much insulin, the cells of the body do not get enough glucose, and your brain is triggered to tell you that you need to eat.
Other
symptoms
Low
blood glucose can also cause nervousness and shakiness, excessive perspiration,
anxiety and weakness.
Symptoms will vary from person
to person, and may be affected by age and sex.
How
self-monitoring of blood glucose (SMBG) helps manage complications of diabetes
When blood glucose levels are poorly controlled, a person with
diabetes will have greater risks of developing other health problems, such as
heart disease, kidney disease, deterioration of vision, nerve problems and
dryness of skin. Regular monitoring can help spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
Heart disease
Diabetes can increase the risk of developing coronary
heart disease, or atherosclerosis. People with diabetes are 2x
more likely to develop heart disease, and people with diabetes are more at risk
of developing cardiovascular complications at an earlier age that can often
result in premature death. Deaths from heart disease in women with diabetes
have increased by 23% over the past 30 years. Compare this to a 27% reduction
in women without diabetes. In addition, deaths from heart disease in men with
diabetes have decreased only by 13%. Compare this to a 36% reduction in men
without diabetes.
In coronary heart disease, a material called plague builds up in the heart's arteries, making them hard and thick, resulting in hardened and narrowed blood vessels that supply blood to the muscle of the heart, and the heart muscle gets less blood and oxygen. With poor blood and oxygen flow to the heart muscle, the heart suffers, and a person may experience many problems, such as:
- Chest pains or
angina
- Heart attack - a
blood clot forms in one of the plague-filled coronary arteries, cuts off
blood supply to the heart, and the heart muscles start to die
- Heart failure -
the heart fails to pump oxygen-rich blood effectively to the blood
- Arrhythmia - the
heart beats irregularly, which could lead to heart failure
Are you at risk of heart disease?
Coronary heart disease is among the leading causes of death in the world. To avoid developing coronary heart disease, you should be aware of risk factors associated with heart disease.
- Manage diabetes
well, including regular self-monitoring of blood glucose.
- Control blood
pressure.
- Do not smoke.
- Drink moderately.
- Eat a healthy
diet, maintain ideal and safe weight.
- Follow a
regularly scheduled exercise program.
- See your doctor
regularly. Get tests that help you and your doctor keep tabs on how well
your heart is doing.
What is atherosclerosis?
Atherosclerosis is
a disease in which deposits of yellowish plaques containing cholesterol, lipid
material, and lipophages (cells that absorb fats) are formed within the
arterial walls.
As these deposits
increase in size, blood flow decreases until there is a complete blockage.
If
the blockage occurs in the vessels supplying blood to the brain, the risk of a
stroke increases.
In
other areas, such as the legs and feet, blockages can lead to tissue death,
resulting in conditions such as gangrene or loss of feeling due to nerve
damage.
Kidney disease
Your kidneys help filter waste
products from your blood and excrete them as urine. You may suffer from nephropathy,
or renal disease, if
you have persistently high blood glucose levels. Diabetes is the leading cause
of end-stage renal disease (kidney failure), resulting in about 43% of new
cases.
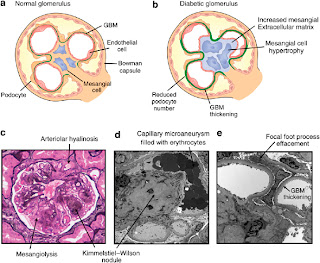 Your doctor may routinely perform tests to detect kidney disease.
Your doctor will perform tests to detect albumin, a protein that leaks into
urine when nephrons stop working properly. He will also check your blood
pressure (the kidneys help maintain normal blood pressure, and high blood
pressure increases the risk of kidney disease). Damage to the nephrons, the
tiny filters in the kidneys, happens gradually, and you and your doctor may
detect kidney problems before they become serious.
Your doctor may routinely perform tests to detect kidney disease.
Your doctor will perform tests to detect albumin, a protein that leaks into
urine when nephrons stop working properly. He will also check your blood
pressure (the kidneys help maintain normal blood pressure, and high blood
pressure increases the risk of kidney disease). Damage to the nephrons, the
tiny filters in the kidneys, happens gradually, and you and your doctor may
detect kidney problems before they become serious.
Regular monitoring can help you spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
Eye Disease
Clouding of vision
Persistent high blood glucose levels harm the eyes, and you could suffer
serious visual impairment, if you fail to control your blood glucose. In fact,
diabetes is the leading cause of new cases of blindness in people aged 20 to 74
years. Each year, up to 24,000 people lose their sight because of diabetes.
 If blood glucose levels are elevated for some time, glucose
crystals can build up on the lens of the eye, resulting in a cataract,
or clouding of the lens. Surgical replacement of the lens with an artificial
one corrects this problem. Your doctor may advise you to have dilated-retina
exams and visual acuity tests every year if you have diabetes.
If blood glucose levels are elevated for some time, glucose
crystals can build up on the lens of the eye, resulting in a cataract,
or clouding of the lens. Surgical replacement of the lens with an artificial
one corrects this problem. Your doctor may advise you to have dilated-retina
exams and visual acuity tests every year if you have diabetes.
Regular monitoring can help you spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
Persistent elevated blood glucose levels damage the blood vessels that feed the
retina, the part of the eye for color vision and detail. This results in fluid
leak into the retina and the growth of new blood vessels and scar tissue,
causing blurring or loss of vision. This type of damage is known as diabetic
retinopathy.
Regular monitoring can help you spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
When on insulin
When you start insulin, you may experience temporary blurring of your eyesight
and other problems. This usually lasts only for a few weeks. Visit your doctor
when it happens.
Regular monitoring can help you spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
Nerve damage
Neuropathies, or
problems of the nerves, are common in those with diabetes. If you have
diabetes, you may suffer nerve damage in different parts of the body. Some
people experience pain, numbness or tingling in the toes, feet, legs, fingers,
hands and arms. Others have shrinking of muscles of the hands and feet, nausea,
vaginal dryness, impotence, diarrhea and indigestion. Nerve problems can also
occur in the organs inside the body. The poorer the blood glucose control, the
higher the likelihood of developing diabetic neuropathy.
Regular monitoring can help you spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
Dry skin
When blood glucose levels are high, your body loses fluid, and
dehydration results in dryness of the skin. When the skin is dry, it can crack
and become vulnerable to skin infections. Also, if you have diabetes, poor
circulation and decreased skin sensation from nerve problems make it difficult
to notice dry skin.
Regular monitoring can help you spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
Infections
High blood glucose levels lower the ability of the immune system
to fight infection. As a result, people with diabetes tend to get infections
more often than those who do not have diabetes, especially when blood glucose
levels are elevated, and poor circulation may cause infections to heal more
slowly. If you have diabetes, you are at risk for infections of the respiratory
system (such as influenza), bladder and kidney infections, disease of the mouth
such as oral candidiasis and gum disease, fungal infections, infections of the
vagina, infections of the skin, and particularly of the foot. In fact, a small
cut on the foot may not heal well and become a focus of serious infections if
not treated well.
Regular monitoring can help you spot patterns to try to avoid high
and low blood glucose, reduce complications of diabetes, and help control your
diabetes.
How can you successfully manage your Diabetes with diet?
Food is one of the main factors that directly impacts blood
glucose levels-and one you can control. There is not one "diabetes
diet" for everyone to follow. Instead, people with diabetes should have a
varied, flexible meal plan based on their lifestyle and personal needs. The key
is knowing how foods, especially the foods you like to eat, impact your blood
glucose levels. As long as you eat a balanced meal plan, you can eat nearly all
of the things you enjoy, at least occasionally.
When you were diagnosed with diabetes, you may have wondered,
"Will I have to give up my favorite foods?" The more you know about
nutrition, the more options you'll realize you have. Your meal plan is not
about depriving yourself of all the things you want; it's about maintaining a
good blood glucose level and eating a well-rounded meal plan. So treat yourself
right by making healthy choices. Your body will feel its best and your blood
glucose is more likely to be in control.
Carbohydrates:
A carbohydrate (or "carb") is a sugar molecule
"chain" that the body uses for fuel. Carbohydrates are found in
nearly every food and include starches, sugars and fiber. All carbohydrates
raise blood glucose levels.
Our bodies convert many food nutrients to glucose, which is the
fuel that runs our bodies. With carbs, this conversion process happens much
faster than with other nutrients - usually within two hours. This is why people
with diabetes have to pay such close attention to foods, and why keeping track
of what you eat can help control blood glucose.
When it comes to glucose control, it may seem as if all carbs are
the same. But for better health and energy, you should choose "high
octane" carbohydrates - those with more vitamins, minerals, and fiber.
Foods like:
- Whole grains,
breads and cereals made from them
- Dried beans,
lentils, and legumes
- Crackers and
cookies with less than 3 grams of fat
- Low-fat or skim
milk and dairy products
- Fresh fruits and
juices and canned fruits made without added sugar
The need for insulin
When you have diabetes, your body either fails to produce enough
insulin, a substance that moves glucose into the cells, or your body responds
poorly to insulin. Over time, your body will produce less and less insulin, and
your blood glucose levels may become more and more difficult to control. To
help you with your diabetes your doctor may prescribe you insulin to help you
control your blood glucose more consistently.
When the body is working well
Starting insulin doesn't mean you've done something wrong or that
you haven't been doing a good job managing your diabetes. Let's look at what
happens in the body when it is working well.
What
happens to your body when you have diabetes?
Replacing the insulin your body needs
By adding insulin to your treatment, your doctor is taking the next step to
help you stay out of the Diabetes Danger Zone. If you have any questions about
your insulin therapy or if you are uncomfortable injecting insulin, talk to
your doctor.
Different types of insulin
and how they work
Some
types of insulin act quickly to match the rise in blood glucose after a meal.
Other types act more slowly to control blood glucose throughout the night and
day. Your doctor will prescribe the insulin that is best for you.
- A basal
insulin dose provides long-lasting control of overnight and
fasting (morning) glucose levels.
- Bolus doses provide
control of more immediate rises in glucose levels. For example, to cover
meals.
- A late-day
basal insulin injection is a common first step in insulin
therapy. Throughout the day your body may still be able to keep your blood
glucose under control with or without diabetes pills. But you may need a
basal insulin injection to help keep your glucose steady throughout the
night.
- A pre-mixed
insulin is a combination of a basal insulin and a fast-acting
insulin that offers the convenience of both precise and consistent dosing.
·
Long acting basal insulin
Insulin type
|
When it starts working
|
When it works at peak
|
How long it lasts
|
|
BASAL
|
Long-acting Usually taken at bedtime
to control glucose while you sleep
|
3 - 4 hours
|
8 - 15 hours
|
22 - 26 hours
|
Intermediate acting Usually taken in the
morning to work all day
|
1 - 3 hours
|
5 - 8 hours
|
Up to 18 hours
|
|
·
When to self-monitor your blood glucose
Insulin type
|
When to self-monitor blood glucose
|
|
BASAL
|
Long-acting Usually taken at bedtime
to control glucose while you sleep
|
Before injecting, to see if your glucose is in the Diabetes Safe
Zone
|
Before breakfast, to see if your insulin dose works to keep you
in the Diabetes Safe Zone throughout the night
|
||
Around 3 a.m. if your fasting results are high or low
|
||
Intermediate acting Usually taken in the
morning to work all day
|
Before injecting, to see if your glucose is in the Diabetes Safe
Zone
|
|
Before and 3 hours after meals, to see if your insulin dose
works to keep you in the Diabetes Safe Zone around mealtimes
|
||
Before bed, to see if you need a snack so your glucose doesn't
fall too low during the night.
|
||
Short acting bolus insulin
Insulin type
|
When it starts working
|
When it works at peak
|
How long it lasts
|
|
BOLUS
|
Short-acting
Sometimes used around mealtimes, it is taken 30 to 45 mins before eating. Therefore, timing of meals is important |
30 - 60 minutes
|
2 - 4 hours
|
5 - 8 hours
|
Rapid acting
Injected right before meals. By the time food is digested and glucose is moving into the bloodstream, rapid-acting insulin is working hard to move glucose into the cells. |
10 - 15 minutes
|
60 - 90 minutes
|
4 - 5 hours
|
|
When to self-monitor your blood glucose
Insulin type
|
When to self-monitor blood glucose
|
|
BOLUS
|
Short-acting
Sometimes used around mealtimes, it is taken 30 to 45 mins before eating. Therefore, timing of meals is important |
Before injecting, to see if your glucose is in the Diabetes Safe
Zone and to help you plan your meal content and insulin dosage
|
2 hours after meals, to check the effect of your insulin dose
|
||
Before bed, to see if you need a snack so your glucose doesn't
fall too low during the night
|
||
Rapid acting
Injected right before meals. By the time food is digested and glucose is moving into the bloodstream, rapid-acting insulin is working hard to move glucose into the cells |
Before injecting, to help determine your insulin dose and to
help you plan your meal content
|
|
2 hours after eating, to check the effect of the insulin dose
|
||
Before bed, to see if you need a snack so your glucose doesn't
fall too low during the night
|
||
Pre-mixed insulin
A pre-mixed insulin is a combination of a basal insulin and a
fast-acting insulin that offers the convenience of fixed precise and consistent
dosing. This may work well in some patients. Its timing of administration, when
it starts working, when it works at peak, and duration of effect depends on the
combination. See characteristics of basal insulin and bolus insulin.
When to self-monitor your blood glucose
Timing of self-monitoring of
blood glucose (SMBG) depends on the combination of basal insulin and bolus
insulin. See characteristics of basal insulin and bolus insulin.






